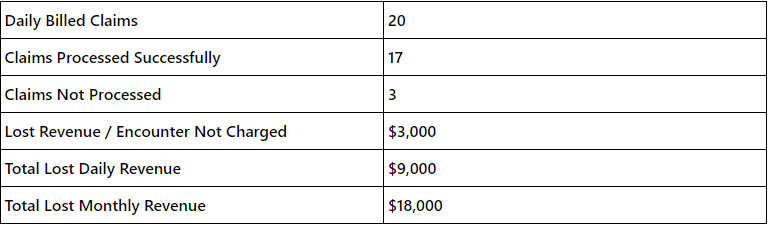
Proven Strategies to Reduce Claim Denials in Your Medical Practice
In the complex world of healthcare, reducing medical claims denials in your medical practice is critical for maintaining operational efficiency and revenue flow. By identifying the most common reasons for claims denials and implementing effective strategies, you can safeguard your practice’s financial health and improve patient care. In this article, we’ll explore proven strategies to help you minimize claim denials, improve your revenue cycle management, and enhance overall operational efficiency.