Out Of Network
Identification and Recovery
Zero Risk. Maximum Reimbursements.
Schedule a quick 15-30 minute call with us for a free consultation to determine your healthcare organization’s needs!
Our Claims Recovery Services
Pre-Payment Recovery: Negotiations Service
Post-Payment Recovery: Appeals Service
Why Choose Us
This Service is HFMA Peer-Reviewed
We Are Success-Based
Decades of Expertise
Largest Healthcare Database
Specialized

This service is Peer Reviewed by HFMA, indicating that we offer a high quality, trustworthy and valuable service for our clients!
* HFMA staff and volunteers determined that these healthcare business solutions have met specific criteria developed under the HFMA Peer Review process. HFMA does not endorse or guarantee the use of these healthcare business solutions or that any results will be obtained.

If you don't get paid on your out-of-network claims, neither do we – which means we work even harder to identify and recover reimbursements on your out-of-network claims. With our no risk approach, it’s a no brainer!

We have over 20 years’ experience in the industry. We’ve built a unique team of experts who worked directly for the largest cost containment vendors and insurance companies, giving us the unique ability to understand their strategies and motives which allows us to stay ahead and get higher payments on bills for our customers. Our team offers advanced workflow processes to successfully navigate the complicated regulation surrounding the reimbursement processes.

To get our high yielding results, we rely on CRXIS, our proprietary data and analytics tool we’ve developed to support us as we go toe-to-toe with payors. CRXIS is the largest health data network in the industry, and helps analyze insurance policies, provides comparable data, and allows us to track the tendencies and trends of the people on the side of the insurance companies and cost-containment vendors.

We don't replace your billing team; we support them behind the scenes! Fighting these claims isn't part of the standard process for any billing team. It's nearly impossible for your staff to dedicate the necessary time and resources to identify, track, and challenge hundreds of claims. Our team has the specialized expertise and data to ensure your billing team can focus on their primary tasks.
Why Choose Us
This Service is HFMA Peer-Reviewed

This service is Peer Reviewed by HFMA, indicating that we offer a high quality, trustworthy and valuable service for our clients!
*HFMA staff and volunteers determined that these healthcare business solutions
have met specific criteria developed under the HFMA Peer Review process.
HFMA does not endorse or guarantee the use of these healthcare business
solutions or that any results will be obtained.
We Are Success-Based

If you don't get paid on your out-of-network claims, neither do we – which means we work even harder to identify and recover reimbursements on your out-of-network claims. With our no risk approach, it’s a no brainer!
Decades of Expertise

We have over 20 years’ experience in the industry. We’ve built a unique team of experts who worked directly for the largest cost containment vendors and insurance companies, giving us the unique ability to understand their strategies and motives which allows us to stay ahead and get higher payments on bills for our customers. Our team offers advanced workflow processes to successfully navigate the complicated regulation surrounding the reimbursement processes.
Largest Healthcare Database

To get our high yielding results, we rely on CRXIS, our proprietary data and analytics tool we’ve developed to support us as we go toe-to-toe with payors. CRXIS is the largest health data network in the industry, and helps analyze insurance policies, provides comparable data, and allows us to track the tendencies and trends of the people on the side of the insurance companies and cost-containment vendors.
Specialized

We don't replace your billing team; we support them behind the scenes! Fighting these claims isn't part of the standard process for any billing team. It's nearly impossible for your staff to dedicate the necessary time and resources to identify, track, and challenge hundreds of claims. Our team has the specialized expertise and data to ensure your billing team can focus on their primary tasks.

If you don't get paid on your out-of-network claims, neither do we – which means we work even harder to identify and recover reimbursements on your out-of-network claims. With our no risk approach, it’s a no brainer!

We have over 20 years’ experience in the industry. We’ve built a unique team of experts who worked directly for the largest cost containment vendors and insurance companies, giving us the unique ability to understand their strategies and motives which allows us to stay ahead and get higher payments on bills for our customers. Our team offers advanced workflow processes to successfully navigate the complicated regulation surrounding the reimbursement processes.

To get our high yielding results, we rely on CRXIS, our proprietary data and analytics tool we’ve developed to support us as we go toe-to-toe with payors. CRXIS is the largest health data network in the industry, and helps analyze insurance policies, provides comparable data, and allows us to track the tendencies and trends of the people on the side of the insurance companies and cost-containment vendors.

We don't replace your billing team; we support them behind the scenes! Fighting these claims isn't part of the standard process for any billing team. It's nearly impossible for your staff to dedicate the necessary time and resources to identify, track, and challenge hundreds of claims. Our team has the specialized expertise and data to ensure your billing team can focus on their primary tasks.
Who We Serve

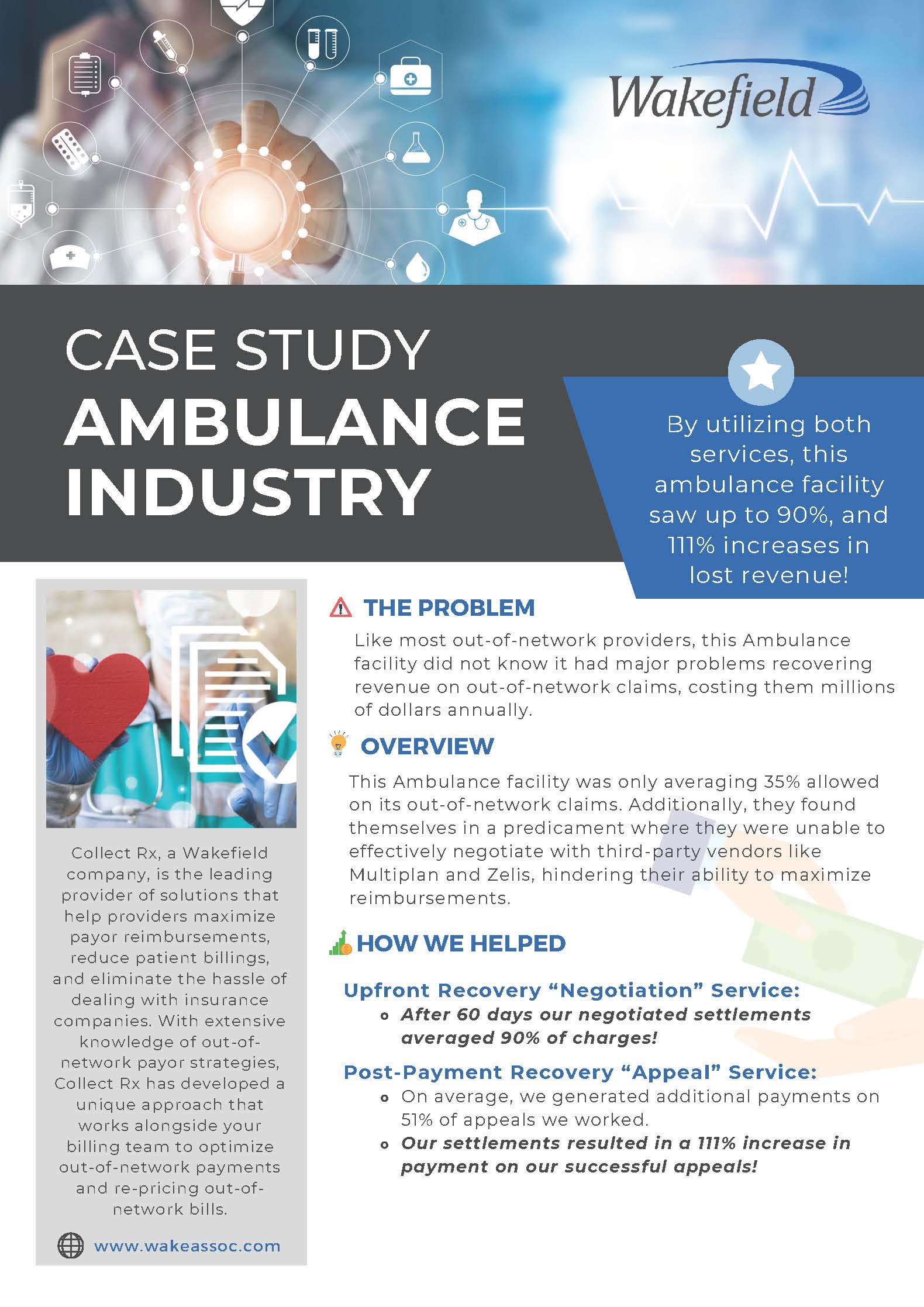
Ambulatory Surgery Centers

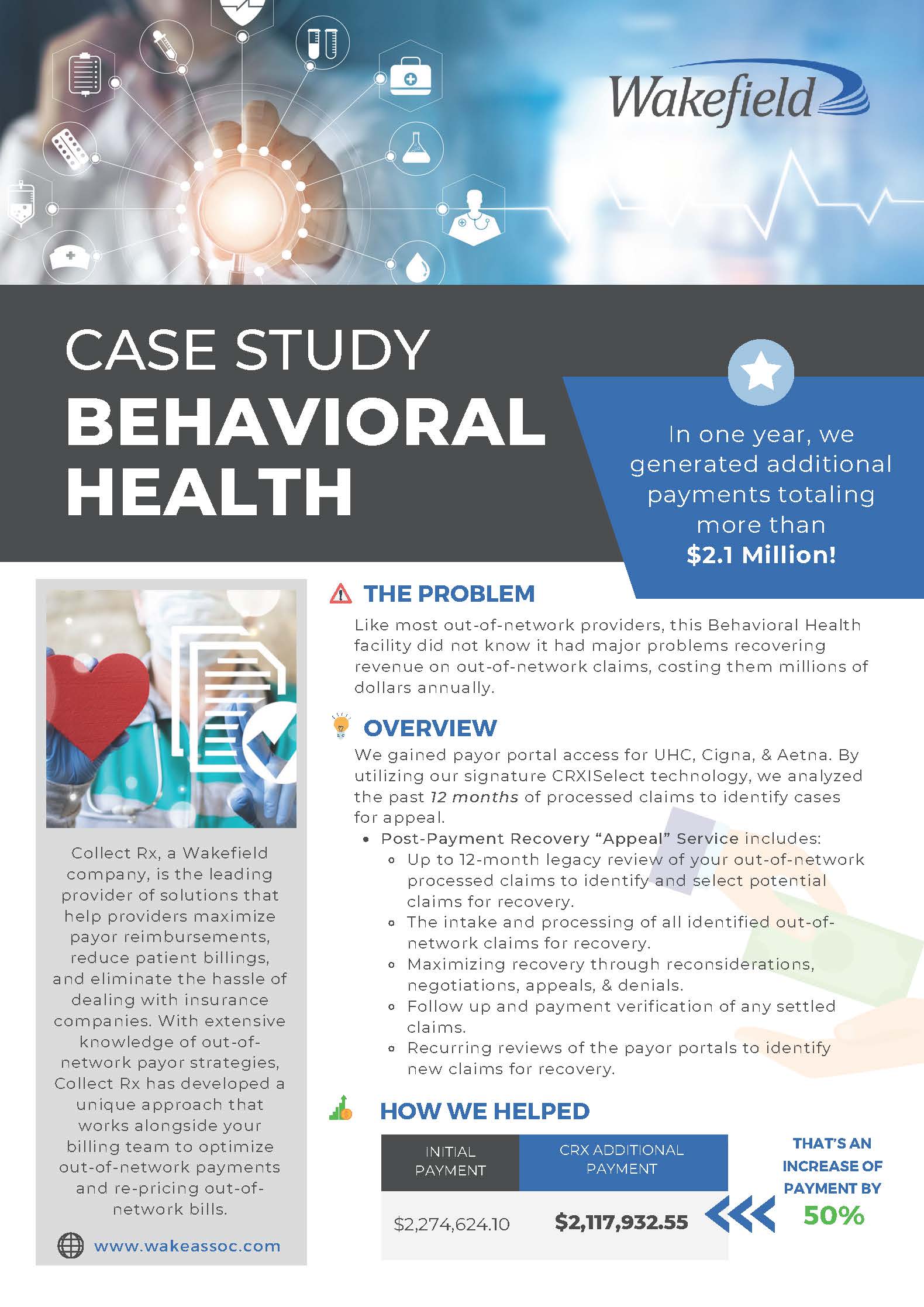
Behavioral Health Providers

Laboratories & Diagnostic Centers

Hospitals

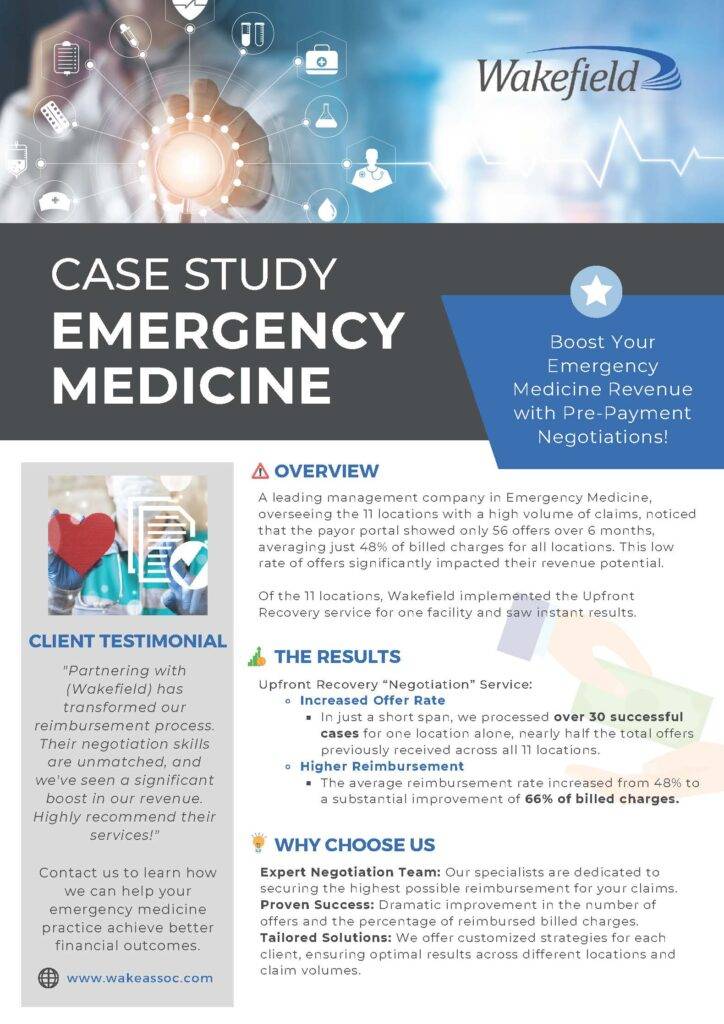
Emergency Medicine

Physician Groups