Proven Strategies to Reduce Claim Denials in Your Medical Practice
Read Time:
- 7
- Minutes
What You’ll Learn:
In this article, you’ll discover key insights into minimizing medical claims denials in your practice. We will cover the most common reasons for claims denials and provide actionable strategies to address them. By the end of the article, you’ll understand how to enhance your revenue cycle management, improve operational efficiency, and safeguard your practice’s financial health, ultimately leading to better patient care and a more streamlined workflow.
Read Time:
- 7
- Minutes
What You’ll Learn:
In this article, you’ll discover key insights into minimizing medical claims denials in your practice. We will cover the most common reasons for claims denials and provide actionable strategies to address them. By the end of the article, you’ll understand how to enhance your revenue cycle management, improve operational efficiency, and safeguard your practice’s financial health, ultimately leading to better patient care and a more streamlined workflow.

Source: Wakefield & Associates

In the complex world of healthcare, reducing medical claims denials in your medical practice is critical for maintaining operational efficiency and revenue flow. By identifying the most common reasons for claims denials and implementing effective strategies, you can safeguard your practice’s financial health and improve patient care. In this article, we’ll explore proven strategies to help you minimize claim denials, improve your revenue cycle management, and enhance overall operational efficiency.
Understanding the Importance of Reducing Claim Denials
Reducing claim denials in your medical practice is essential to ensure your revenue cycle remains uninterrupted. Frequent denials can lead to cash flow issues and hinder net patient revenue, resulting in lost opportunities for growth.
Additionally, minimizing denied claims improves your practice’s efficiency and allows staff to focus more on patient care instead of dealing with complex appeals and resubmissions. By addressing claim denials early, your practice can achieve better financial outcomes.
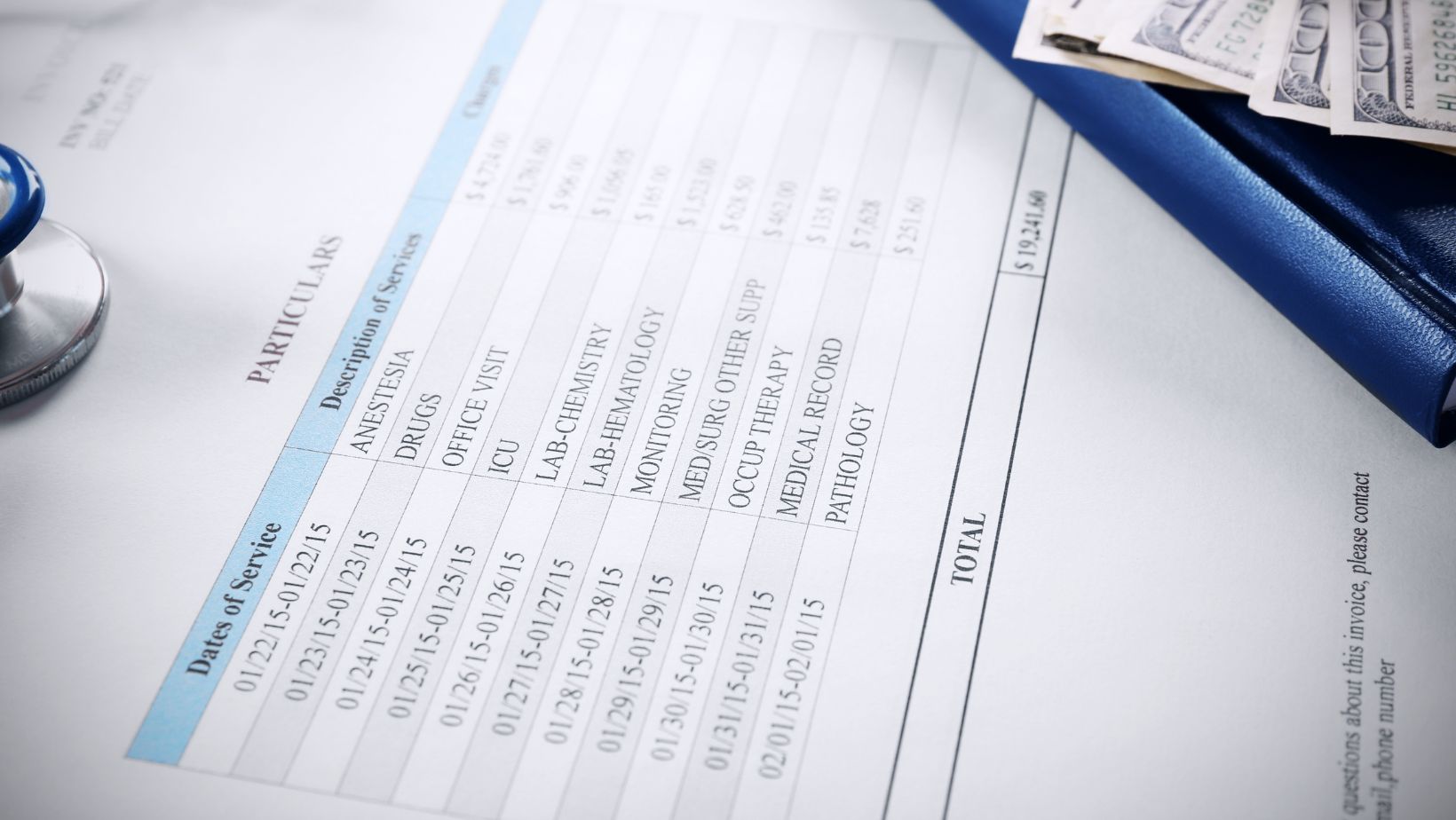
Common Reasons for Initial Medical Billing Denials
Understanding the root causes of initial medical billing denials is the first step toward reducing them. One frequent issue involves insurance eligibility response errors, where coverage isn’t verified correctly.
Other common causes include missing information, such as a social security number or payer rules violations like submitting claims with wrong plan codes. Identifying these causes can help you prevent future denials.
Prior Authorization Challenges and Solutions

One major factor contributing to denied claims is the lack of prior authorizations. Medical practices often face challenges with insurance companies requiring prior authorization for certain healthcare services.
To mitigate this, streamline your process by automating eligibility verification and ensuring patient information is up to date before services are rendered. This step can reduce your denial rates significantly.
The Role of Medical Necessity in Denials
Many medical billing denials arise from the failure to meet medical necessity requirements. Insurance companies often reject claims they deem unnecessary for the clinical outcomes requested.
To prevent this, ensure that your medical records are complete and clearly document the medical necessity of procedures. This will help avoid soft denials and ensure claims are processed efficiently.
Optimizing Revenue Cycle Management to Reduce Denials
An optimized revenue cycle is crucial to reducing denials. The Medical Group Management Association (MGMA) poll indicated a significant average increase in denials, highlighting the challenges healthcare organizations face. By improving your medical billing processes and tracking denial trends, you can identify patterns that lead to denials.
Effective revenue cycle management involves regular auditing of your billing practices, as well as ensuring that claims meet payer requirements from the start.
Clean Claims: A Critical Component to Avoid Denials
Submitting clean claims is key to minimizing technical errors that result in denials. Simple mistakes like missing a modifier or coding a service under the wrong plan code can lead to rejections.
By ensuring that all details on the claim form are accurate and complete, you improve your chances of getting claims approved on the first try.
Categorizing Denials for Better Insight
To tackle denial rates effectively, it’s important to categorize denials based on common types such as coverage issues, technical errors, or incomplete documentation.
This process helps you identify root causes and address specific areas of concern, reducing the likelihood of future denials.
Leveraging Denial Data to Improve Compliance
Denial data is a valuable resource for improving both compliance and operational efficiency. Regularly analyzing denial trends allows you to identify areas where payer rules are frequently violated.
By addressing these gaps, your practice can reduce denials, improve compliance, and ultimately boost cash flow and overall revenue.
Enhancing Data Quality to Minimize Claim Errors
Improving data quality is essential to reducing errors in claim submissions. Ensure that patient and procedure data is accurate before submitting claims to reduce rejections due to coverage issues or incomplete records.
Training staff to check details and verify insurance eligibility upfront will help minimize claim errors, reduce backlogs, and increase overall efficiency.
The Benefits of Identifying Denial Trends
Regularly identifying and analyzing denial trends can have a direct impact on your practice’s bottom line. Tracking denial rates and pinpointing the most common issues, such as missing information or incorrect coding, can help reduce the frequency of rejected claims.
By staying proactive, you can implement corrective measures that lead to fewer denials and improved financial stability.
Prioritize Eligibility Verification
Make eligibility verification a priority to avoid unnecessary claim denials related to insurance coverage. This step ensures that the patient’s information is up to date and helps avoid coverage issues.
Identify Root Causes of Denials
Analyzing denial data regularly helps you identify the root causes of recurring claim denials, allowing you to implement targeted solutions for improvement.
Improve Compliance with Payer Requirements
Ensure that your staff is well-trained on payer requirements to reduce claim denials related to non-compliance. This can help improve both cash flow and patient satisfaction.
Monitor Denial Trends for Better Efficiency
Tracking denial trends allows you to identify common errors and inefficiencies in your medical billing processes, helping to reduce denial rates.
Submit Claims on Time
Submitting claims in a timely manner is essential for avoiding late claims and other issues that could result in denials. Create a workflow that prioritizes timely submission.
Utilize Denial Data to Improve Operations
Leverage the power of your denial data to improve operations across the board. Data-driven insights can help pinpoint areas for improvement in claim submission.
Enhance Communication with Staff
Ensure that staff members are regularly updated and trained on evolving payer requirements to minimize claim denials and maintain compliance.
Focus on Clean Claims for Faster Processing
Submitting clean claims with accurate, complete information leads to faster processing and fewer denials due to technical errors or missing documentation.
Streamline Case Management Processes
By streamlining your case management process and making sure all required documentation is available, you can reduce the chances of denied claims due to missing information.
Review Denial Rates Monthly
Regularly review your denial rates and take corrective actions to reduce future denials. Proactive monitoring and adjustments can greatly enhance overall efficiency.
By implementing these strategies, your medical practice can effectively minimize claim denials, streamline your revenue cycle, and ensure a smoother experience for both your staff and patients.
Accurate Coding and Billing Practices
Accurate coding and billing practices are crucial in reducing claim denials and ensuring timely reimbursement for healthcare services. Inaccurate coding can lead to denied claims, delayed payments, and even audits. Here are some tips to ensure accurate coding and billing practices:
Regular Training for Staff: Ensure that your billing and coding staff receive regular training to stay updated with the latest coding standards and payer requirements. This can help prevent errors that lead to claim denials.
Use Updated Coding Manuals: Always use the most current coding manuals and resources. Outdated codes can result in denied claims, so it’s essential to stay current with coding updates and changes.
Conduct Periodic Audits: Regularly audit your billing and coding processes to identify and correct errors. This proactive approach can help you catch mistakes before they result in denied claims.
Implement Quality Control Measures: Establish quality control measures to review claims before submission. This can include double-checking codes, verifying patient information, and ensuring all required documentation is included.
By prioritizing accurate coding and billing practices, your medical practice can significantly reduce claim denials and improve overall revenue cycle management.
Table of Contents
- FAQs
- Reduce Claim Denials in Your Medical Practice
What are the most common reasons for claim denials?
The most common reasons for claim denials include insurance eligibility response errors, incomplete or missing information, failure to obtain prior authorization, and issues with medical necessity documentation. Technical errors, such as coding mistakes or submitting claims with the wrong plan code, can also lead to denied claims.
How can we reduce claim denials in our practice?
To effectively reduce claim denials, your practice should implement eligibility verification upfront, ensure accurate and complete documentation of medical necessity, and streamline the process for obtaining prior authorizations. Additionally, submitting clean claims free of technical errors and regularly reviewing denial data to address root causes can help minimize rejections.
How long does it take to see results from improving our claim submission process?
Notable improvements in reducing claim denials typically become evident within 3 to 6 months, depending on the complexity of your billing processes and how quickly changes are implemented. During this period, regularly track and analyze denial trends to make ongoing adjustments and improve efficiency.
What is the difference between hard denials and soft denials?
Soft denials refer to claims that are denied but can be corrected and resubmitted, usually due to minor errors or missing information. Hard denials, on the other hand, cannot be resubmitted and result in lost revenue unless appealed. Understanding the differences can help your team prioritize corrections and prevent future denials.
Why is it important to track and categorize denials?
Tracking and categorizing denials allows your practice to identify denial trends and pinpoint areas that need improvement, such as recurring payer rule violations or missing patient information. By addressing these issues proactively, you can reduce future denials, improve cash flow, and enhance your practice’s overall financial health.
- Latest News

Wakefield Receives HFMA Peer Review Designation
Navigating the complex landscape of legal concepts for complex claims can be daunting. This comprehensive blog, based on a recent webinar hosted by Becker’s Health Care, aims to shed light on critical aspects of this subject.

Mastering Legal Concepts for Complex and Problem Claims: A Comprehensive Guide
Navigating the complex landscape of legal concepts for complex claims can be daunting. This comprehensive blog, based on a recent webinar hosted by Becker’s Health Care, aims to shed light on critical aspects of this subject.

10 Strategies for Effective Revenue Cycle Management In Healthcare
Discover how simplifying healthcare billing can transform the future of medical finances. Learn about the latest trends, technologies, and strategies for efficient healthcare cost management and patient billing solutions.

Introduction to Accounts Receivable in Medical Billing
Discover how simplifying healthcare billing can transform the future of medical finances. Learn about the latest trends, technologies, and strategies for efficient healthcare cost management and patient billing solutions.
Simplifying Healthcare Billing: Navigating the Future of Medical Finances
Discover how simplifying healthcare billing can transform the future of medical finances. Learn about the latest trends, technologies, and strategies for efficient healthcare cost management and patient billing solutions.
